The provision of adequate and affordable health care services for Nigerians, now about 177,5 million, has been a major challenge for federal, state and local governments in the country. The development of modern health care facilities requires substantial financial resources and is an essential component of national health policy. The preservation of the gains made in health care delivery is important otherwise there would be reversals that could lead to the resurgence of some of the diseases that have been brought under control. The Federal Government has therefore made it a priority to put in place a robust national health policy that is predicated not only on the development of public health care facilities across the country, but also on the creation of an enabling environment for private health care facilities to thrive and provide affordable health care services, while at the same time recognising the importance of traditional medicine.
MAJOR HEALTH PROBLEMS
Several factors are largely responsible for the common diseases found in Nigeria.
These include its tropical location, its level of economic development, and lifestyle.
Nigeria is located in the tropics and this is responsible for the prevalence of tropical diseases in the country.
Futhermore, as a developing country, it is also confronted with diseases associated with poverty, illiteracy, ignorance and poor hygiene and sanitation.
The other diseases are those that are found in all climates and in all countries, irrespective of their levels of development and some of them are referred to as lifestyle diseases.
The tropical diseases include malaria, yaws, sleeping sickness, filarial diseases, guinea worm and yellow fever.
Climatic conditions in the tropics are conducive for the propagation of the agents or vectors of these diseases. The diseases associated with poor hygiene and sanitation include diseases of the typhus group, leprosy and relapsing fever.
Finally, the diseases that are independent of climate and level of development include measles, sexually transmitted diseases, pneumonia, heart disease, chicken pox and tuberculosis. In July 2014, the ebola virus disease that is ravaging some West African countries was brought into Nigeria by an infected individual who flew into Lagos from one of the affected countries.
The federal and state governments responded to the emergency very swiftly and, fortunately, so to say, the fatalities were limited to 7 out of 19 cases. All those infected were people who had primary or secondary contact with index case (ie. the initially infected traveller). Fourty two days after the outbreak, the World Health Organisation (WHO) declared Nigeria Ebola-Free (on 20 October 2014).
The preceding tables support the contention that tropical diseases, diseases of poverty and diseases that are independent of climate or geographical location are present in Nigeria. Besides, and more importantly, the tables indicate that the major health problems in Nigeria are preventable.
This being the case, preventive medicine rather than curative medicine should be the main thrust of the country’s health policy.
NATIONAL HEALTH POLICY
Policy Articulation
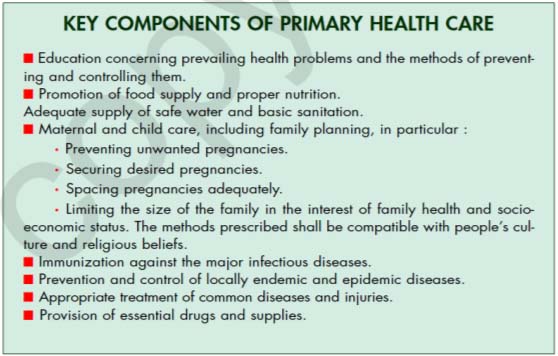
Primary health care (PHC) is the foundation of Nigeria’s health policy, the tenets of which include the following, among others:
• The Federal, State and Local Governments and the private health sector of Nigeria commit themselves and all the people to intensive action to attain the goal of health for all citizens, that is, a level of health that will permit them to lead socially and economically productive lives at the highest possible level.
• All governments of the federation are convinced that the health of the people not only
contributes to better quality of lives but is also essential for the sustained economic and social development of the country as a whole.
• The people of this nation have the right to participate individually and collectively in the planning and implementation of their health care. However, this is not only their right, but also their solemn duty.
• Primary health care is the key to attaining the goal of health for all the people of this
country.
Although PHC is central, the national health care system is developed at three levels, namely, Primary Health Care (PHC), Secondary Health Care (SHC) and Tertiary Health Care (THC). The health policy document states that the “The Federal, State and Local Governments shall support in a coordinated manner a three tiered system of health care.
Essential features of the system shall be its comprehensive nature, multi sectoral inputs, community involvement and collaboration with non-governmental providers of health care. The policy envisages public participation in planning and implementation as well as partnership with the private sector, voluntary agencies and local communities.
Primary Health Care (PHC)
PHC is key to the attainment of Nigeria’s health policy goals.
In line with the Alma Ata Declaration (WHO, URSS- 1978), government defines PHC as follows:
“PHC is essential health care based on practical, scientifically sound and socially acceptable methods and technology made universally accessible to individuals and families in the community through their full involvement and at a cost that the community and state can afford to maintain at every stage of their development in the spirit of self-reliance. It shall form an integral part of the national health system of which its central function and main focus is the overall social and economic development of the community. It is the first level of contact of individuals, the family and community with the national health system, bringing health care as close as possible to where people live and work, and it constitutes the first element of a continuing health care process.”
The Role of Traditional Medicine
Nigeria’s PHC has a place for traditional medicine and its practitioners. This is in recognition of two basic realities. First and foremost, access to modern health care services is relatively limited, especially in rural areas. Secondly, traditional healers are more widely available, their practices are compatible with local cultures, and there is hardly any social distance between practitioner and patient. For these reasons, traditional healers now have some official recognition.
Therefore, the health policy requires that local health authorities shall, where applicable, seek the collaboration of traditional practitioner’s in promoting their health programmes.
Traditional health practitioners shall be trained to improve their skills and to ensure their cooperation in making use of the referral system in dealing with high risk patients.
The Revised National Health Policy (2004) captures this policy thrust as follows: “Due to the age-long importance of traditional medicine and new trends in health care delivery, coupled with the reality that a high proportion of Nigerians patronize traditional health practitioners, there is a need to integrate the practice with orthodox medicine by ensuring the establishment of minimum standards for the practice”.
Hospitals
While the main thrust of PHC is preventive medicine, hospitals are primarily concerned with curative medicine. The hospitals in Nigeria fall into two main categories, namely, Secondary Health Care (SHC) facilities (or General Hospitals), and Tertiary Health Care (THC) facilities. Over the years, more resources have been devoted to curative medicine than preventive medicine, even though the latter is more cost effective.
The current emphasis on PHC is meant to correct this imbalance. All the same, SHC and THC facilities remain dominant features of Nigeria’s health care delivery system. General Hospitals are probably the most important and most common type of SHC facilities in the country. SHC facilities offer curative and other services that are beyond the capacity of PHC facilities to provide. In fact, they serve as referral centres for PHC facilities. There are, of course, other facilities that provide secondary health care services. These include maternity centres, clinics and health centres.
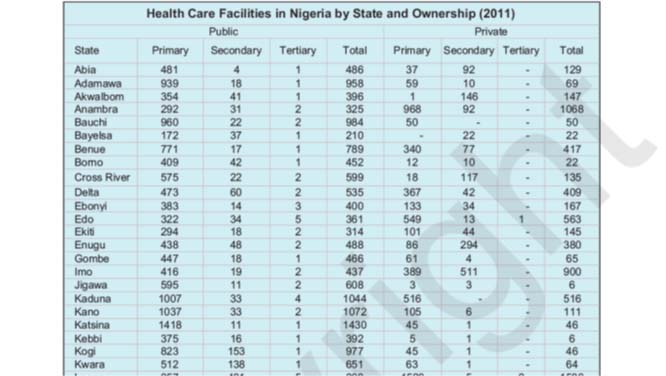
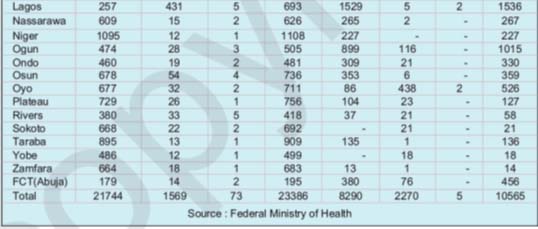
The distribution of PHC, SHC and THC facilities in Nigeria by state and ownership are set out in the following table.
Nigeria has 30,034 PHC facilities, 3,839 SHC facilities and 78 THC facilities. Most of these facilities are owned by government. The private providers include voluntary agencies religious groups, private individuals and communities.
Private providers feature prominently in the provision of SHC facilities: general hospitals, clinics, health centres, maternity centres and so on, especially in urban centres.
This locational pattern of the private facilities is understandable, given the importance of the profit motive in the locational decisions of their proprietors.
The table also shows that the health care facilities in the country are reasonably well distributed geographically. This is especially the case with government-owned facilities.
The private health care facilities are more unevenly distributed among the states than the public ones. The THC facilities are highly specialized facilities and they provide specialized services of the sort that cannot be provided by the SHC facilities.
In fact, the THC facilities are referral centres for SHC facilities to which the latter refer difficult cases.
Training Facilities
Some of the THC facilities serve as the teaching hospitals of the medical schools in some Nigerian universities. In addition to providing specialized services, the teaching hospitals are used to train doctors, dentists and other categories of medical and paramedical personnel.
Thus, some of the teaching hospitals have schools of nursing, schools of midwifery, and other institutions that train paramedics. The training of paramedics is not done by teaching hospitals alone as there are other institutions which train them. Nursing schools are cases in point. They are mostly owned by governments and voluntary agencies.
Data from ‘Social Statistics in Nigeria 2012’, a publication by the National Bureau of Statistics (NBS) show that in 2011, there were 10,275 doctors and 553 dentists in Nigeria. These numbers are questionable given the fact that only recently (August 2014) 16,000 resident doctors in federal tertiary hospitals were relieved of their appointments. This number does not include other categories of doctors as well as doctors in state government hospitals, private hospitals and voluntary agency/missionary hospitals. Also the NBS, in one of its previous publications reported 30,885 doctors and 2,221 dentists in the year 2000.
The oldest teaching hospital in Nigeria is the University College Hospital (UCH), Ibadan. Other notable ones include Lagos University Teaching Hospital (LUTH), Lagos, Ahmadu Bello University Teaching Hospital (ABUTH), Kaduna, University of Nigeria Teaching Hospital (UNTH), Enugu, Obafemi Awolowo University Teaching Hospital (OAUTH), Ile-Ife, University of Benin Teaching Hospital (UBTH), Benin City, University of Port Harcourt Teaching Hospital (UPTH), Port Harcourt, University of Calabar Teaching Hospital (UCTH), Calabar and University of Maiduguri Teaching Hospital (UMTH), Maiduguri. All of these are affiliated with federal universities. Some state universities and private universities also have teaching hospitals.
Examples include Delta State University, Olabisi Onabanjo University (Ogun State), Ambrose Ali University ( Edo State), Benue State University, Lagos State University, and Igbinedion University (private), among others. In all, there are about 20 teaching hospitals in the country, and more are being established as some universities add medicine to their curricula. It is important to stress that not all THC facilities are teaching hospitals.
It is clear from the foregoing that the most prevalent diseases in Nigeria are preventable and are therefore relatively easy to manage. This informs the emphasis on PHC which is essentially a preventive health care strategy. It also informs the aggressive immunization programmes that federal, state and local governments are implementing across the country.
The provision of potable water is part of the effort by government to ensure that the incidence of water-borne and water-related diseases is minimized.
It will also facilitate the maintenance of personal hygiene and sanitation. The provision of potable water is one of the key components of government’s PHC programme.
In addition to PHC facilities, the federal and state governments as well as voluntary agencies and private individuals have established SHC and THC facilities in different parts of the country to provide higher order health care services.


